Managing Hip Pain and Sciatica Linked to SI Joint Issues
Anatomy Of The Sacroiliac Joint
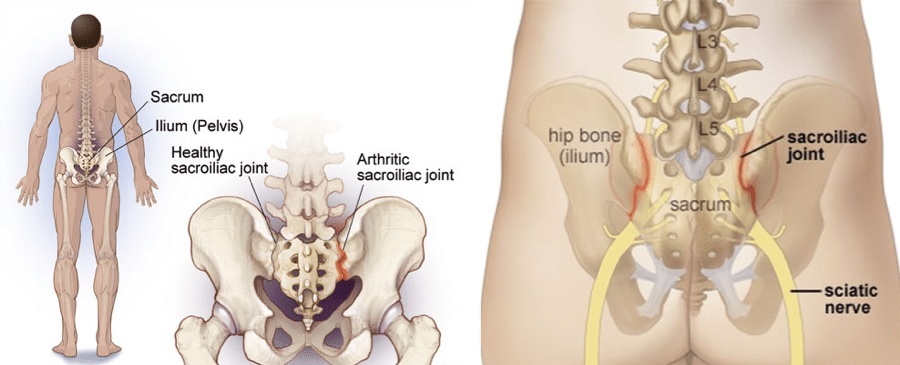
The sacroiliac (SI) joint is the linchpin connecting your spine to your pelvis. It links the sacrum, that triangular bone at your spine’s base, to the iliac bones in your pelvis.
This joint isn’t your everyday hinge; it’s a true synovial joint with irregular, ear-shaped surfaces that fit snugly together. This unique shape helps resist sliding forces, giving you a solid foundation to stand and move.
Biomechanics And Stability
Think of the SI joint as a well-guarded poker hand—it moves deliberately, with less than 4 degrees of rotation and about 1.6 mm of sliding. Its stability is all about compression, held tight by strong ligaments and muscle contractions.
Key muscles like the transversus abdominis and pelvic floor group pull their weight in keeping the joint steady, preventing unwanted shifts that could spell trouble.
Typical Movements And Relation To Hip Pain
The SI joint’s main job is to spread out the forces from your upper body down through your hips and legs. When this joint gets unstable or inflamed, it’s like a dealer who messed up the shuffle—your load transfer gets misdirected.
That misfire can irritate nearby nerves, including those that run into your hip and down your leg, creating pain that looks a lot like sciatica, even if the problem isn’t your spine per se.
Sacroiliac Joint Concept Map
Level 1: SI-Joint Anatomy
Level 2: Biomechanics (limited rotation, compression-based stability)
Level 3: Pathology (instability, hyper/hypomobility)
Level 4: Symptoms (hip/buttock pain, sciatica-like leg pain)
Common Causes And Risk Factors For SI Joint-Related Hip Pain And Sciatica
When the sacroiliac joint acts up, it's usually due to a handful of usual suspects:
- Dysfunction – either the joint is moving too much or not enough.
- Inflammation – often from overuse or injury, causing irritations around the joint.
- Trauma – a fall, accident, or any direct hit to the pelvis or lower back.
- Degenerative Changes – wear and tear that comes with age or repetitive stress.
- Biomechanical Imbalances – uneven leg length or muscular imbalances that throw the joint off kilter.
Certain players in this game are at higher risk:
- Women often have more ligament laxity, especially around childbirth, increasing joint movement.
- People with a history of trauma to the pelvic or lower back area.
- Jobs requiring heavy lifting or repetitive twisting motions.
- Those with leg length discrepancies or unusual gait patterns.
How SI Joint Dysfunction Produces Sciatic And Hip Pain Pathophysiology Explained
Nerve Irritation Mechanisms
When the SI joint loses its tight grip, it disrupts how force flows through your pelvis and lumbar spine. This instability squeezes or irritates nearby nerve roots, especially those contributing to the sciatic nerve.
That’s the fast break causing pain signals to shoot down from your buttock into your thigh and leg.
Inflammation Patterns
Inflamed tissues in and around the SI joint act like a bad referee, sending mixed signals to your nervous system. The irritation causes swelling and sensitizes nerves, making even small movements painful.
Referred Pain Symptoms
Pain from SI joint dysfunction isn’t always local. It often masquerades as classic sciatica by radiating down the leg, or as deep hip pain. Knowing this helps avoid costly misreads that send you chasing the wrong diagnosis.
SI Joint Dysfunction Pain Progression
SI Joint Instability or Inflammation
↓
Nerve Root Irritation (Lumbosacral Roots)
↓
Referred Pain To Hip, Buttock, And Leg
↓
Symptoms Mimicking Sciatica
If you’re battling hip or sciatica-like pain, think about where the fault lines run. Sometimes the answer’s not in the spine but in this underappreciated joint.
For daily support, especially during recovery or flare-ups, a quality hip brace can help reduce strain and boost stability without slowing you down.
Diagnosing SI Joint-Related Hip Pain and Sciatica Accurately
Let’s cut to the chase: diagnosing SI joint issues ain’t like calling a straight flush every time. The sacroiliac joint is a tricky little player hiding behind hip and low back pain, often masquerading as lumbar spine or hip problems. The first step? Knowing how to distinguish SI joint pain from other suspects.
Clinical Examination and Pain Provocation Tests
The clinical exam is your opening hand. It relies on specific pain provocation tests that challenge the SI joint’s stability and irritability. Tests like the FABER (Flexion, Abduction, External Rotation) or the Gaenslen's test push the joint just enough to see if it lights up the patient’s pain.
No single test seals the deal, so the smart money is on a combination—if a few tests come back positive, odds are good SI joint dysfunction is in play. These tests aren’t foolproof, though, because pain patterns overlap with hip or lumbar root issues.
Imaging: What Cards to Play
Now, imaging—X-rays, MRI, CT scans—are your table’s chips, but they don’t always tell the full story. Standard X-rays can show joint degeneration or trauma but often miss subtle instability. MRIs are great to spot inflammation or soft tissue issues surrounding the SI joint but aren’t definitive for joint dysfunction itself.
CT scans give detailed bone structure views, useful if you suspect fractures or advanced degenerative changes. Yet, none of these are slam-dunks for diagnosing SI joint pain alone. They’re more valuable to rule out other hip or spine conditions.
Diagnostic SI Joint Injections: The Ace Up Your Sleeve
If you want to be sure, a diagnostic SI joint injection is where the game changes. This involves injecting a local anesthetic directly into the SI joint under imaging guidance to see if the pain temporarily disappears.
Think of it like a poker tell—if the pain goes away, you just nailed the SI joint as the culprit. If not, look elsewhere for the pain source. This procedure has higher accuracy than clinical tests or imaging alone but is more invasive and not without risks.
Differential Diagnosis: Don’t Fold Too Soon
One of the biggest traps is assuming all hip or leg pain comes from the SI joint. Lumbar spine disorders like herniated discs or facet arthritis and hip joint problems like labral tears can mimic SI joint symptoms.
That’s why a solid diagnosis always includes ruling out these other conditions. You wouldn’t sit at a blackjack table ignoring the dealer’s card, would you? Treating the wrong source wastes time and chips.
Conservative Treatment Options: Physical Therapy, Exercises, and Lifestyle Adjustments
If your SI joint’s throwing you a curveball, starting with conservative treatment is the smart play. Physical therapy targets those muscles and ligaments around the joint to stabilize the pelvis and ease stress.
Here’s a playbook to follow in your rehab grind:
- Targeted physical therapy focusing on stabilizing muscles like the transversus abdominis and pelvic floor. These guys lock down the joint, giving it some much-needed support.
- Strengthening exercises for hips and lower back to improve load distribution.
- Stretching tight muscles — hamstrings, hip flexors — these can pull the pelvis out of line and crank up pain.
- Posture correction to avoid putting unnecessary shear forces on the SI joint.
- Lifestyle tweaks, like managing body weight and reducing repetitive motions that nag the joint.
Stick with it—that’s the unglamorous but essential part. Patients who bail out early don’t win. Small victories like improved mobility and less pain come from consistent effort, not magic pills.
Interventional Therapies: Injections and Minimally Invasive Procedures
When conservative tactics aren’t cutting it, injections and minimally invasive treatments step into the ring. Corticosteroid injections target inflammation head-on, often reducing pain and improving function for weeks to months.
Then there’s PRP—injecting platelet-rich plasma from your own blood to encourage healing. It’s like dealing yourself a better hand, though evidence is still catching up on who benefits most.
Prolotherapy aims to strengthen ligaments by provoking a mild inflammatory response, encouraging tissue repair. It’s a more long-game strategy compared to steroids.
Radiofrequency ablation (RFA) is next-level. By using heat to disrupt nerve signals causing pain, it can provide relief lasting several months. Not everyone’s a candidate, though—typically, folks who respond well to diagnostic injections but still have pain are up for this.
Each option has its table stakes—knowing who benefits and who folds early comes down to a good conversation with your healthcare provider. Sometimes you gotta roll with the conservative bets before upping the ante.
Patient Outcomes and Safety Profiles Across Treatment Options
Let’s cut to the chase: when you’re sidelined by SI joint pain that’s shooting down your hip and leg, what really matters is how much you're gonna improve—and how safe the treatment is while doing it.
Patient-reported outcomes like Visual Analog Scale (VAS) scores and the Oswestry Disability Index (ODI) give us the real-world scorecard on pain relief and function.
From what we’ve seen, conservative care including physical therapy offers decent relief, with many patients reporting moderate drops in VAS scores and improvements in ODI without the risk blacklist attached to surgery or injections.
Injection Therapies: Quick Fix or Slow Play?
Injections—steroids, PRP, or prolotherapy—are the pit stops where you hope for fast pain relief. Satisfaction rates hover fairly high: patients often see drops in VAS scores by a point or two. But like bluffing in poker, sometimes it works and sometimes it doesn’t hold up.
Adverse events? Low but not zero. Infection, nerve irritation, or temporary flare-ups come from real deals with injections. Luckily, registries say complications stay in the low-single-digit percentages.
Radiofrequency Ablation: Cutting the Pain, Not the Corner
RFA takes out those pesky nerve signals with precision, slashing pain sustainably in patients unresponsive to injections. VAS reductions and ODI improvements tend to outswing injections, with decent patient satisfaction.
Adverse events are rare but can include temporary numbness or localized discomfort. For players looking to avoid the big surgery gamble, RFA is a solid middle-ground play.
Surgical Fusion: The Full Table Play
When all else fails, surgical fusion aims to lock down that unstable joint and end the pain game for good. Patients who go this route often show the biggest gains in VAS and ODI scores, especially in refractory cases.
The catch? Surgery comes with higher risks — infection, nerve damage, implant issues — so it’s like going all-in with a marginal hand. The adverse event rates are noticeably higher versus injections or RFA.
Advances and Emerging Therapies for SI Joint-Related Hip Pain and Sciatica
Forget the same old playbook: new treatment options are coming in hot for SI joint pain and sciatica. Let’s talk neuromodulation, biologics, and next-gen implants—tactics designed to raise your odds without stacking more risk on the table.
Neuromodulation: Rewiring the Pain Signal
Picture this: a device subtly tweaking nerve signals to dial down pain without cutting anything out. Neuromodulation for SI joint pain is gaining traction as a less invasive but effective way to modify how your nerves report pain.
Clinical trials suggest this approach can decrease VAS scores significantly and improve patient satisfaction, especially when standard treatments don’t hold. Regulatory bodies are watching closely, with approvals picking up pace in some states.
Biologics: Healing From the Inside Out
The buzz on biologics like platelet-rich plasma (PRP) and stem cell therapies is more than just smoke. These treatments aim to jump-start the body’s own repair crews within the joint, addressing inflammation and tissue quality.
While the jury’s still out on long-term outcomes compared to traditional injections, early studies show promising reductions in pain scores and improved function. Expect more clinical trials to drop soon that’ll clarify their place on the table.
Minimally Invasive Stabilization Devices
Next up: a newer wave of “small incision, big impact” devices designed to stabilize the SI joint without the heavy artillery of classic fusion surgery.
Manufacturers are pushing slimmer hardware options that promise fewer complications and faster recovery. Early adopters report high patient satisfaction and solid pain relief, setting the stage for wider adoption.
Clinical Trials and Regulatory Moves
Across the country, multiple clinical trials chase FDA approval on fresh options. Some states are warming up with new insurance coverage policies reflecting these innovations.
If you’re keeping score, emerging treatments could shake up pain management strategies widely—making the future feel less like a shot in the dark and more like a calculated bet.
Practical Tips for Managing Pain and Improving Mobility at Home
If you’re holding down the fort with SI joint or sciatica pain, managing the situation at home is key to staying in the game longer and avoiding costly trips to the ER.
Here’s the playbook for staying mobile and comfortable without overdoing it:
- Heat and Ice Therapy: Alternate ice packs to reduce inflammation and heat pads to relax tight muscles. Aim for sessions around 15 minutes each.
- Safe Movement: Avoid sudden twists or heavy lifting. When standing or sitting, maintain good posture to keep joint stress low.
- Assistive Devices: Use a cane or walker if needed to offload pressure from the painful side. Even a lumbar support belt can add stability.
- Gentle Stretching: Calf, hamstring, and lower back stretches help relieve tension that can radiate from the SI joint.
- Regular Walks: Short, frequent walks keep blood flowing and muscles active without overloading the joint.
Do these moves right, and you can chip away at discomfort without calling in the pros too quickly.
When to Seek Medical Help: Warning Signs and Follow-Up Recommendations
Don’t Play With Fire: Red Flags You Can’t Ignore
Not all SI joint pain is created equal. Some symptoms mean you need to see a doc right away—no waiting for Monday morning.
- Worsening numbness or weakness in the legs or feet (think: dropped foot or loss of balance).
- Loss of bowel or bladder control.
- Severe, unrelenting pain that won’t ease with rest or usual care.
- Signs of infection: fever, redness, or swelling around the joint.
Follow-Up: Don’t Ghost Your Provider
Once SI joint dysfunction is on your radar, keeping regular follow-up appointments keeps you from getting caught on the ropes.
Your care team will want to monitor symptoms and adjust treatments. If pain or function dips, that’s your cue to check back in.
Consistency here is like sticking to a solid poker strategy—it’s what keeps you winning in the long haul.
Summary of Key Points and Managing Expectations for Recovery
SI joint-related hip pain and sciatica don’t always play fair. Some folks get quick relief; others wrestle with persistent symptoms.
Understand this: recovery times vary widely, and patience is part of the game. It’s not always a clean cut win—but a marathon where small improvements accumulate.
Multidisciplinary care—PT, medical management, injections, or surgery—is your best bet for staying ahead.
Your engagement is the kingpin here. Show up for yourself, work with your care team, and avoid rash all-ins that could cost you more down the road.
Manage your expectations, keep your eyes on the chips on the table, and remember: this isn’t about a one-hand knockout—it’s about playing smart, steady, and long.

